
The prevalence of diabetes in the U.S. is growing. The CDC reports that more than 100 million U.S. adults are now living with diabetes or prediabetes. That’s one in 10 Americans who have diabetes, and one in three with prediabetes.
The trends of the general population impact the number of patients who require glycemic management care as inpatients. And because inpatient diabetes care is challenging and expensive, the trends point toward a hard road ahead for healthcare providers.
But despite evidence that measuring quality and providing feedback or incentives for providers improves diabetes care, many health systems don’t actively track metrics related to glycemic management (glucometrics).
In fact, quality teams often don’t become aware of glycemic management performance until something goes wrong, like a hypoglycemic incident.
In this article, we’ll show you how to get started with tracking and analyzing glucometrics in order to improve the quality of diabetes care at your health system.
The most fundamental metrics related to the quality of inpatient diabetes care are the incidence of severe hypoglycemia (BGs <40 mg/dL), moderate hypoglycemia (BGs <70 mg/dL) and severe hyperglycemia (BGs >300 mg/dL).
These glucometrics should be tracked across all patients receiving insulin or receiving a certain number of blood glucose checks — not just patients diagnosed with diabetes. Doing so may ensure you don’t miss undiagnosed cases and patients who receive insulin due to stress-related hyperglycemia, such as those undergoing CABG surgery.
But how do you measure the incidence of hypo- and hyperglycemia?
Each of these methods has value, but it’s important to understand their shortcomings.
For example, percent of point-of-care blood glucose values might be skewed by differences in testing frequency between patients and between units. Meanwhile, percent of patient stays could be skewed by patients with widely varying lengths of stay.
While it’s not perfect, percent of patient days is, in most cases, the most clinically meaningful method for tracking glycemic management performance in inpatient settings.
I recommend this paper from the Society of Hospital Medicine for more good information about calculating glucometrics.
Many hospitals rely on clinicians to report instances of hypo- and hyperglycemia themselves, which doesn’t usually provide reliable data.
One strategy to begin collecting glucometrics in a more structured way is by setting up automated reports in your EMR. Most systems allow users to set up reports that pull data from patient charts and present it for analysis.
However, these automated reports may be missing data or contain duplicate information, so it’s critical to ensure your data is clean before using the results to inform decision making.
Ultimately, the most effective way to reliably track and report on glucometrics with clean data is to use a purpose-built technology solution. Glytec’s eGlycemic Management System (eGMS) includes built-in glucometrics reporting.
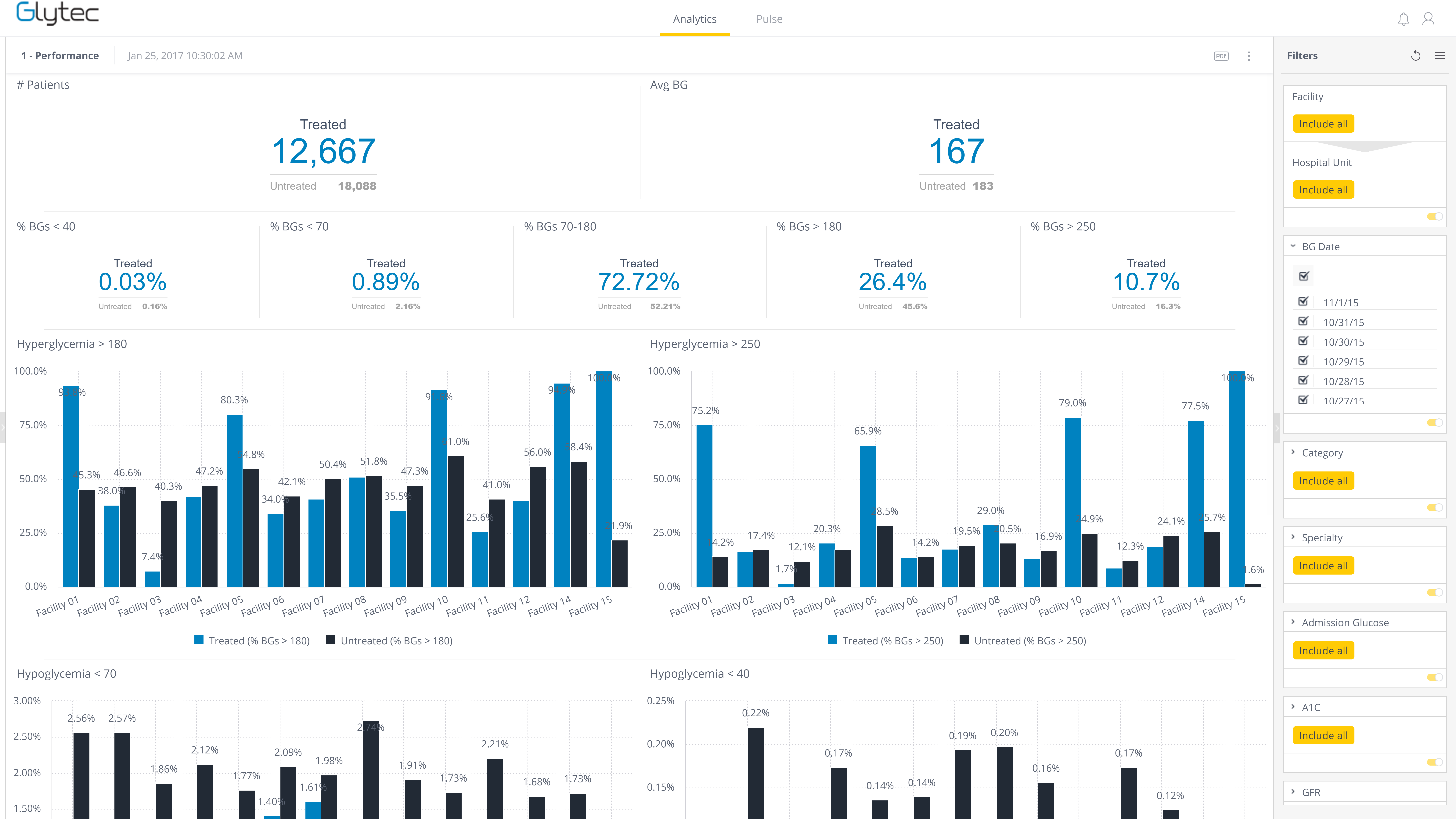
Providers use the system to input blood glucose values and other patient data in order to calculate personalized insulin dosing recommendations. eGMS also syncs with the EMR and laboratory interface. Using these datasets, eGMS automatically creates a dashboard of important glucometrics, with the ability to drill deeper with custom reports.
Further reading: How Glytec’s eGMS Unlocks Quality Improvements in Glycemic Management
Tracking the incidence of hypo- and hyperglycemia is a good place to begin with glucometrics.
Once you have a system in place for collecting and tracking reliable, accurate information about your health system’s glycemic management performance, you can then begin analyzing the data for deeper insights.
You might break down your blood glucose analysis into smaller ranges for more detailed observations. Maybe you’d like to break down results by hospital or unit, or by patient information such as renal status, diagnosis, history of diabetes or BMI.
You could also track other measures directly related to diabetes care, such as:
If you use a near-real-time dashboard like the one in Glytec’s eGMS, you can also use glucometrics for proactive quality management efforts. For example, if a provider’s patients are experiencing hyperglycemia rates above a certain threshold, the quality team can intervene to determine where the issue lies.
You can’t manage what you can’t measure. But when you start tracking and analyzing glucometrics, you can measurably improve the quality of diabetes care at your health system.
Reliable glucometrics also allow quality teams to secure buy-in from hospital leadership for QI initiatives and improve adoption among providers by showcasing how new strategies and therapies can measurably improve patient safety, which translates to return on investment of both time and money.
Glytec offers a high-reliability strategy for improving glycemic management performance, and we can also help you benchmark your current performance to kick-start your quality improvement journey.
ECO #0966-A

©2024 Glytec, LLC | Terms of Use | Legal Disclaimer | Privacy Policy | Contraindications, Warnings and Precautions
The eGlycemic Management System® is a modularized solution for glycemic management across the care continuum that includes Glucommander®. Glucommander® is a prescription-only software medical device for glycemic management intended to evaluate current as well as cumulative patient blood glucose values coupled with patient information including age, weight and height, and, based on the aggregate of these measurement parameters, whether one or many, recommend an IV dosage of insulin, glucose or saline or a subcutaneous basal and bolus insulin dosing recommendation to adjust and maintain the blood glucose level towards a configurable physician- determined target range. Glucommander® is indicated for use in adult and pediatric (ages 2-17 years) patients. The measurements and calculations generated are intended to be used by qualified and trained medical personnel in evaluating patient conditions in conjunction with clinical history, symptoms, and other diagnostic measurements, as well as the medical professional’s clinical judgement. No medical decision should be based solely on the recommended guidance provided by this software program.
Glucommander® is only available for use in the United States.
This site is only intended for use in the United States.