Hospital Pharmacy Resources for Safe & Effective Insulin Management

Insulin is a high-alert medication: errors associated with both intravenous (IV) and subcutaneous (subQ) insulin can seriously impact patient safety.
Hospital pharmacists have a responsibility to improve the effectiveness and safety of insulin dosing management. This can be accomplished both by decreasing errors using safety precautions and by promoting the adoption of standard-of-care glycemic management among providers.
To assist hospital pharmacists in achieving this goal, Glytec has compiled data and resources related to insulin safety risks and their effects, common safety precautions and glycemic management standards.
To ask a question related to insulin management or to recommend an addition or improvement to this resource, please contact us.
The Dangers of Insulin
Insulin is considered a “high-alert” medication by the Institute for Safe Medication Practices (ISMP), meaning it bears a heightened risk of causing significant patient harm when used erroneously.
Errors involving insulin can lead to hyperglycemia and hypoglycemia, as well as serious outcomes such as confusion, seizures, coma or death.
- In a 2014 survey from ISMP, pharmacists and nurses ranked IV insulin as the No. 1 drug of most concern out of 39 high-alert medications, directly above anticoagulants and chemotherapeutic agents.
- In the same survey, respondents ranked subQ insulin as the No. 9 drug of most concern.
- Insulin is involved in 16.3% of medication error reports for high-alert medications, more than any other medication type.
- The Centers for Medicare & Medicaid Services (CMS) considers patient death or serious disability associated with hypoglycemia a “never event” and may withhold reimbursement for these incidents.
The far-reaching effects of poor glycemic management
In addition to having a direct impact on patient health, hypo- and hyperglycemia associated with insulin errors and poor glycemic management have been shown to impact key hospital quality indicators including readmissions, length of stay, and mortality:
One study of 43,659 patients shows that those who experienced severe hypoglycemia had a 61.5% higher readmission rate, stayed in the hospital an average of 6.6 days longer and had a mortality rate almost three times that of patients who stayed in normal range.
More results:
| Group | Average LOS (#Days) Per Patient |
Readmission Rate | Mortality Rate | Average Cost Per Patient Stay |
| Severe hypoglycemia (<40 mg/dL) | 14.4 | 21.8% | 9.2% | $21,444 |
| Moderate hypoglycemia (40-69 mg/dL) | 11.6 | 18.2% | 5.2% | $16,456 |
| Normal glycemia (70-180 mg/dL) | 7.8 | 13.5% | 3.2% | $11,039 |
| Severe hyperglycemia (>300 mg/dL) | 8.6 | 16.1% | 3.6% | $11,711 |
FURTHER READING
Hidden Costs of Poor Glycemic Management: Readmissions, LOS & Mortality
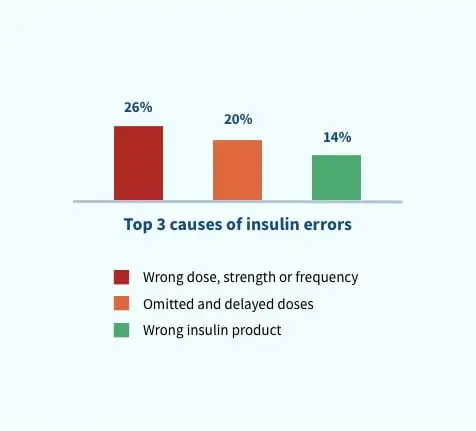
Types and causes of insulin errors
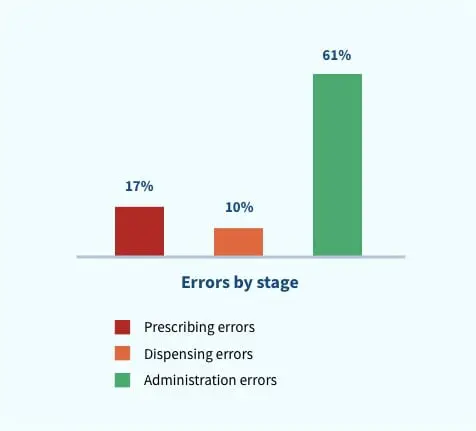
![]()
According to the report, incidents of wrong dose, strength or frequency were caused by factors including:
- Incorrect prescription on admission
- Abbreviation of “units”: The abbreviations “U” and “IU,” when written in poor handwriting, may be misread as “0” or “10”
- Incorrect monitoring of blood glucose and dose adjustment of insulin
- Poor documentation of dose administration
- Duplicate dose administration
- Errors in the calculation of insulin doses for intravenous infusion
- Incorrect programming of electronic infusion devices
![]()
Incidents of omitted and delayed insulin doses resulted from:
- Incorrect prescription on admission
- Abbreviation of “units”: The abbreviations “U” and “IU,” when written in poor handwriting, may be misread as “0” or “10”
- Incorrect monitoring of blood glucose and dose adjustment of insulin
- Poor documentation of dose administration
- Duplicate dose administration
- Errors in the calculation of insulin doses for intravenous infusion
- Incorrect programming of electronic infusion devices
Meanwhile, incidents of administering the wrong insulin product resulted from mixing up the similar-sounding proprietary names of medications, e.g. Humalog and Humulin.
Common IV insulin safety precautions
To address the risks of errors involving insulin, many hospital pharmacies adopt, develop and promote safety precautions.
According to a 2019 survey from Pharmacy Practice News, common safety precautions and practices for IV insulin include:
- Only 1 standard insulin drip concentration product
- Insulin drip must be placed on a smart IV pump for administration
- Independent nurse double check at bedside before starting infusion
- Patient ID label applied in pharmacy
- All insulin drips ordered from preestablished order sets
- Pharmacist must visually verify dose of insulin before injection into IV piggyback
- High-alert medication label applied in pharmacy to bag
- Compounded using IV workflow program using barcode scanning and documentation
- Segregated storage in the pharmacy
- IV-line label placed for insulin drips
- Not available on override from ADC
- Patient ID label applied on nursing unit
- Segregated storage on unit

While these safety precautions are critical, they don’t address ineffective practices at the prescription stage. The use of sliding scale insulin and confusing paper protocols by providers can lead to ineffective care even when safety guidelines are followed because they don’t take into account patients’ unique responsiveness to the medication.
Pharmacy leaders can promote comprehensive insulin safety by advocating for the adoption of computerized order entry technologies and standard-of-care dosing decision support among providers.
IV Insulin: Pharmacy’s Role in Reducing Risks
Risks and safety precautions for subcutaneous insulin
In a 2014 ISMP survey, pharmacists and nurses ranked subQ insulin as the No. 9 drug of most concern out of 39 high-alert medications, and ranked it in last place compared to the others when asked how confident they were in their safety precautions.
To help address this gap, ISMP published guidelines for optimizing safe subcutaneous insulin use in adults in 2017.
According to the ISMP guidelines, the following have been identified as targeted priority areas of risk concerning subQ insulin:
- Errors and poor outcomes with sliding scale insulin dosing
- Variable or absent insulin standard order sets
- Intermediate and long-acting subQ insulin doses not dispensed in the most ready-to-use form in inpatient settings
- Errors with communicating and measuring doses of concentrated insulin
- Poor coordination of insulin with meals and glucose monitoring in inpatient settings
- Lack of protocols to guide insulin administration
- Lack of prospective risk assessment to identify patients at high risk for hypoglycemia
- Lack of prospective risk assessment to identify patients at high risk for hyperglycemia
- Misuse of insulin pen devices
- Misuse of insulin syringes, needles and vials
- Miscommunication of blood glucose values in inpatient settings
- Lack of patient education
The ISMP goes on to provide a detailed list of safety guidelines. Read the full list in their report.
Use of an eGlycemic Management System® can help address many of these priority risk areas using technology.
How eGMS Improves Administration of SubQ Insulin for Inpatients
Glycemic management standard of care
Preventing errors in the dispensing and administration of insulin is just one way pharmacists can improve glycemic management at their hospitals. To truly minimize risks, pharmacists should also understand and promote standard-of-care glycemic management practices.
Standard recommendations for patients that need insulin therapy:
How Glytec can help
Glytec’s eGlycemic Management System (eGMS) is a comprehensive technology solution that addresses the complex processes, risks and challenges surrounding glycemic control.
eGMS centers on Glucommander™, FDA-cleared software that delivers personalized insulin dosing recommendations at the point of care.
A few key ways that eGMS can help healthcare providers include:
![]()
Improving glycemic management:
eGMS has been proven to decrease time to target blood glucose and significantly reduce the incidence of hypoglycemia and hyperglycemia.
![]()
Improving adoption of standard-of-care basal-bolus insulin dosing:
One hospital’s use of eGMS helped the facility improve basal-bolus insulin utilization from 5% to 96%.
![]()
Decreasing errors in insulin administration:
One hospital’s implementation of eGMS resulted in a reduction of preventable hypoglycemia-related adverse drug events by 62.6%.

Additional resources
For more information about glycemic management and insulin safety, visit:
- Institute for Safe Medication Practices (ISMP)
- American Association of Clinical Endocrinologists (AACE)
- American Diabetes Association (ADA)
- International Society for Pediatric and Adolescent Diabetes (ISPAD)
- Joslin Diabetes Center
- Juvenile Diabetes Research Foundation (JDRF)
- Sansum Diabetes Research Institute