
For many hospital leaders, glycemic management isn’t a priority. While they know that hypo- and hyperglycemia negatively affect patients, they’re usually unaware that these conditions are also having a massive impact on the bottom line.
One problem with one-size-fits-all protocols for insulin dosing — beyond the fact that they’re potentially dangerous — is that they don’t provide data on the effectiveness of glycemic management across the organization. And no data means hospital leadership can’t see the relationship between glycemic management performance and organizational KPIs.
But poor glycemic management can be a huge driver of costs and negative patient outcomes for hospitals, including readmissions, length of stay and mortality.
Here, we’ll take a look at what one hospital system and one academic medical center learned when they investigated glycemic management performance, and what similar organizations can do to reduce hospital readmissions, length of stay and hospital mortality rates.
To better understand the financial impact of poor glucose control in hospitalized patients, the diabetes leadership team at Florida Hospital System (now AdventHealth Orlando) evaluated the prevalence and risk of hypo- and hyperglycemia, comparing glucose data to national benchmarks.
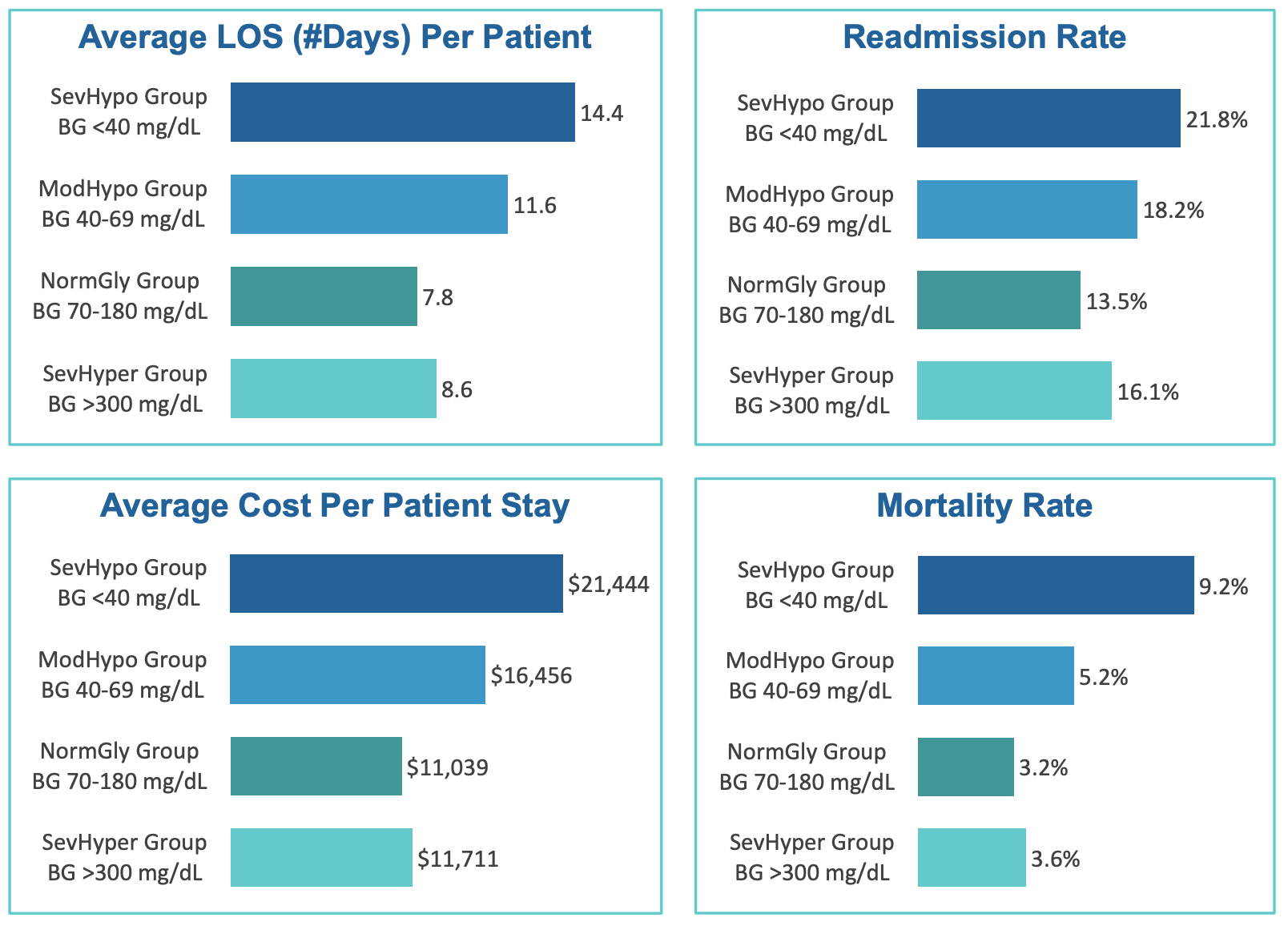
The study, “Financial Implications of Poor Glycemic Management & Improvement Strategies for Optimal Outcomes,” classified point-of-care blood glucose data into four groups: severe hypoglycemia, moderate hypoglycemia, normal glycemia and severe hyperglycemia.
Correlations between blood glucose data and mortality rates, length of stay, readmissions and hospital costs were analyzed for each group.
The authors learned that patients in all groups other than normal glycemia had higher mortality rates, longer hospital stays and more frequent readmissions than the rest of the patient population.
The difference was greatest in the severe hypoglycemia group. These patients had a 61.5% higher readmission rate, stayed in the hospital 6.6 days longer on average, and had a mortality rate nearly three times that of normal glycemia patients.
Additionally, severe hypoglycemia had a significant impact on financial outcomes, increasing the total cost of care by nearly $7.7 million over the 12-month period of the study.
The research also found that patients with severe hypoglycemia incurred an average cost per stay $10,405 higher than those with normal glycemia.
To safely convert from sliding scale insulin therapy to basal-bolus insulin therapy, Kaweah Delta Medical Center in Visalia, California implemented Glytec’s eGlycemic Management System® (eGMS).
In a study of the results, the center compared the standard IV insulin therapy and subcutaneous (SubQ) insulin usual care to nurse-directed, computer-guided Glucommander™, an FDA-cleared insulin dosing decision support module of eGMS that’s integrated with the medical center’s EHR system.
Comparing Glucommander to usual care, Kaweah Delta saw 2,434 fewer hypoglycemic events, resulting in savings of $7,141,356 over the first year, or $2,934 per hypoglycemic event.
Kaweah Delta reduced the average length of stay by 1.67 days, which accounts for savings over the first year of $2,579,200.
The results of these two studies make it clear that there is a deep relationship between glycemic management and the hospital’s bottom line. Strategies to reduce incidences of hypo- and hyperglycemia are crucial for patient safety and quality of care, as well as long-term clinical and operational excellence.
Understanding this can help hospitals reduce hospital readmissions, length of stay and mortality rates.
In a webinar hosted by the American Hospital Association, Dr. Richard Pratley of AdventHealth Orlando and Dr. Steven Edelman of the University of California San Diego discussed the results of the Florida Hospital System research, and how reducing hypoglycemia risks can improve the quality and cost of care for those who require insulin therapy.
Pratley notes six particular steps that the Florida Hospital System took based on their learnings, which ultimately reduced severe hypoglycemia in their hospitals by 40 to 95% over paper-based protocols.
For those looking to reduce hospital readmissions, length of stay and mortality rates, monitoring and improving glycemic management is key.
Glytec’s eGlycemic Management Software can help hospital leaders gain more insight into glycemic management performance and improve that performance to achieve better outcomes.
#0844-A

©2024 Glytec, LLC | Terms of Use | Legal Disclaimer | Privacy Policy | Contraindications, Warnings and Precautions
The eGlycemic Management System® is a modularized solution for glycemic management across the care continuum that includes Glucommander®. Glucommander® is a prescription-only software medical device for glycemic management intended to evaluate current as well as cumulative patient blood glucose values coupled with patient information including age, weight and height, and, based on the aggregate of these measurement parameters, whether one or many, recommend an IV dosage of insulin, glucose or saline or a subcutaneous basal and bolus insulin dosing recommendation to adjust and maintain the blood glucose level towards a configurable physician- determined target range. Glucommander® is indicated for use in adult and pediatric (ages 2-17 years) patients. The measurements and calculations generated are intended to be used by qualified and trained medical personnel in evaluating patient conditions in conjunction with clinical history, symptoms, and other diagnostic measurements, as well as the medical professional’s clinical judgement. No medical decision should be based solely on the recommended guidance provided by this software program.
Glucommander® is only available for use in the United States.
This site is only intended for use in the United States.