The Frequency of Hypoglycemia in Hospitalized Patients Treated With Insulin Increases Overall Costs Associated with Hospitalization and Length of Stay
Presentation
American Diabetes Association Scientific Sessions
Date
June 2016
Authors
Joseph Aloi,1 Jagdeesh Ullal,2 Amy Henderson,3 Raymie McFarland3
BACKGROUND
Hyperglycemia during hospitalization is associated with poor patient outcomes, as well as increased costs, due to impact on length of stay, surgical complications and 30-day readmissions. Hospital associated hypoglycemia also drives inpatient associated complications and therefore cost, but little data exists on the actual financial implications associated with inpatient hypoglycemia.
METHODS
The aim for this study was to examine the association of incidence and severity of hypoglycemia for patients prescribed insulin during a hospitalization with length of stay (LOS) and overall cost of the inpatient stay.
This study evaluated 46,744 patients admitted to a single academic medical center during a 1-year period with hyperglycemia and who were prescribed insulin during the hospitalization.
Data analysis was abstracted to compare LOS and overall cost of inpatient stay for patients who were on insulin and experienced a severe hypoglycemic event (SHE) (BG <50 mg/dL; n = 387) to patients that did not experience significant hypoglycemia during the admission (n = 46,744).
| SHE | Patients, n (%) |
|---|---|
| 1 | 195 (50.5%) |
| 2 | 94 (24.4%) |
| 3 | 36 (9.3%) |
| 4 | 24 (6.2%) |
| >4 | 37 (9.6%) |
RESULTS
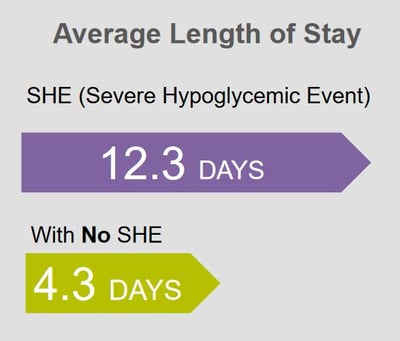
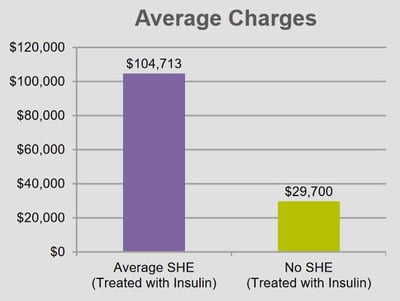
As a group, patients with SHE had increased LOS (12.3 vs. 4.3 days) and higher overall costs ($104,713 vs. $29,700) compared to patients with diabetes treated with insulin without a SHE. Frequency of hypoglycemia was also associated with increasing costs and LOS such that more than 3 SHE increased LOS an additional 4 days (14.4 days) and increased associated costs for the admission an additional $94,948.
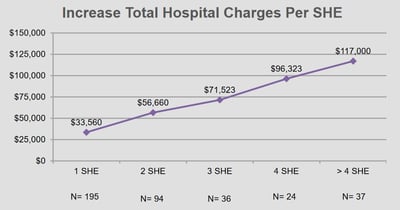
Patients with an admission diagnosis of diabetes treated with insulin during hospitalization that experience at least one SHE have higher associated costs of hospitalization and LOS compared to similar patients without a SHE. Each incremental SHE increased total hospital charges by (1 SHE $33,560 2 SHE $56,660, 3 SHE $71,523 , 4 SHE $96,323, and >4 SHE $117,000).
Increase in hospital charges: 1 SHE was $6,544,200, 2 SHE $5,326,040, 3 SHE $2,574,828, 4 SHE $2,311,752 & >4 SHE $4,329,000. Total increase in hospital cost for the 387 SHE patients was $21,085,820.
The average age for patients with an SHE was 59.9 years and with an average BMI of 28.9.
CONCLUSION
These data support an association between inpatient hypoglycemia and increased costs of care mostly attributable to increasing LOS. Further prospective studies are needed to clarify the association and identify strategies to prevent hypoglycemia and possibly lower costs for hospitals and health care systems.
Affiliations
- Wake Forest School of Medicine, Winston Salem, North Carolina.
- Eastern Virginia Medical School, Norfolk, Virginia.
- Glytec, Waltham, Massachusetts.