Presentation
Association of Diabetes Care & Education Specialists Annual Conference 2021
Date
August 12th, 2021
Authors
Jordan Messler, MD, SFHM, FACP, Kerri Doucette, BSN, RN, RDN, CDCES
WHY DATA MATTERS
- Change is hard: data can make it easier
- Can’t improve what you can’t measure
- Regulatory measures are coming
How Data Overcomes Barriers to Change
- Allows Real Time Changes: Measure-Vention
- Provides Benchmarks to compare and show success
- Achieves Situational Awareness
- Creates a sense of Urgency
- Fosters Transparency
- Creates Accountability
- Can show Improvement over time
- Allow for Standardization to show variation
- When done well, can provide Storytelling With Data
How to Measure What You Want to Improve
- What is your goal?
- Who is your audience?
- What are you trying to improve?
- Which data should you capture?
- How will data help improve the user journey?
- What are the (internal & external) benchmarks?
- Can you use the data to diagnose the problem?
- Can you use the data to develop a solution?
The Time is Now: Regulatory Measures Are Coming
PROPOSED CMS MEASURES as of 7/2021
Severe Hypoglycemia (NQF #3503e)
- % of patients having >1 BG < 40 mg/dl during their hospital stay, within 24 hours of an antihyperglycemic agent (insulin)
Severe Hyperglycemia (NQF# 3533e)
- % of patient days with >1 BG > 300 mg/dl, exclude first/last partial days
- Inpatients with diabetes, receiving >1 dose of insulin (or any anti-diabetic medication) or any BG >200
Types of Glycemic Success Measures
Structure
- Multidisciplinary Glycemic Committee
- Champions (nursing, physician, pharmacy)
- Regular Meetings
Outcomes
- Glucometrics
- Clinical (surgical site infections, complications, mortality)
- Financial (LOS, Costs per Case)
Process
- Insulinometrics
- Ordering practices
- Workflows: meal-time triad, BG timeliness checks
- HbA1c ordering
Balancing
- Hypoglycemia compared to hyperglycemia
- LOS compared to readmissions
MEASURE-VENTION: Allows Real-Time Change
- A high-reliability strategy via active surveillance
- Identifies and measures outcomes at time of care
- Create ability to intervene in real time
- Improvement interventions are applied directly from performance measurement
Examples:
- Daily Report of <100 mg/dl pushed to front-line resource (nurse, CDCES, charge nurse, provider) can foster warnings that encourage insulin order change to prevent hypoglycemia
- Daily Report of <70 mg/dl can help address root causes in real time
GLUCOMETRICS: Inpatient Blood Glucose Data Analysis Methodologies
Example: assume 10 patients, 5 days each, 4 BGs per day
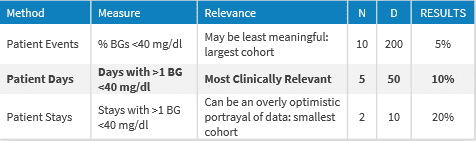
Data should be able to be filtered by Health System, Hospital, Unit (ICU vs non-ICU) and provider group, as well as by renal function, type of diabetes, A1c.
INSULINOMETRICS: Insulin Therapy Ordering Practices’ Impact on Glycemic Control
Inpatient insulin therapy data help to understand the ordering practices of physicians and the administering practices of nurses and how they impact glycemic control. Evaluating, sharing and responding to this data can drive best practice changes and safer care.
Insulin factors to evaluate include:
- Insulin order set type (Sliding scale vs Basal, bolus plus correction)
- Dose edits
- Timing of insulin
- Number of patients treated on insulin who meet criteria
- Duration before starting insulin treatment
- Insulin starting doses compared to home doses
- Withholding insulin
BENCHMARKS: Apples to Apples or Apples to Oranges?
Currently, comparing glycemic data from hospital to hospital is challenging since different criteria may be used and there are no agreed-upon benchmark measurements. If the latest CMS glycemic measures are approved in 2021, this will set a new standard of care.
When comparing your data with other facilities, consider:
-
Are the same metrics being evaluated? (ex. Patient Day vs Patient Event)
-
Is the same exclusion criteria used? (some datasets exclude DKA or Day 1 data)
-
Are the same populations being compared? (ICU vs Med-Surg, Renal vs Post-Cardiac surgery
References
- Bersoux, S., Cook, C. B., Kongable, G. L., Shu, J., & Zito, D. R. (2014). Benchmarking Glycemic Control In U.S. Hospitals. Endocrine Practice, 20(9), 876-883.
- Thompson, B. M., & Cook, C. B. (2017). Glucometrics and Insulinometrics. Current Diabetes Reports, 17(12). doi:10.1007/s11892-017-0964-2
- Curtiss Cook, Beth Elias, Gail Kongable, Daniel Potter, Katherine Shepherd, and David McMahon (2010) Diabetes and Hyperglycemia Quality Improvement Efforts in Hospitals in the United States: Current Status, Practice Variation, and Barriers to Implementation. Endocrine Practice: March 2010, Vol. 16, No. 2, pp. 219-230.
MAR-0000355 Rev 1.0