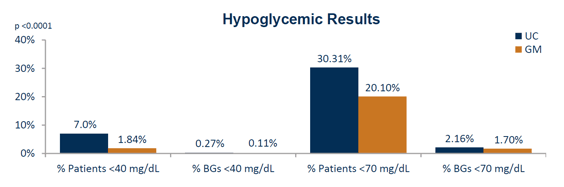
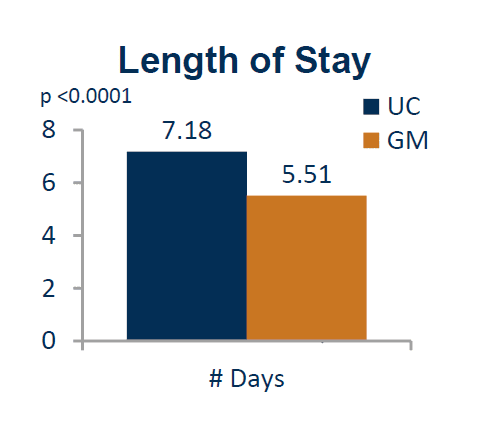
Reduction in Hypoglycemic Events: 2,434 fewer hypoglycemic events with GM versus UC, resulting in savings of $7,141,356 over the first year, or $2,934 per event. Reduction in Average Length of Stay: 1.67 fewer days, resulting in savings over the first year of $2,579,200
Presentation
American Diabetes Association Scientific Sessions
Date
June 2017
Authors
Rosalina Newsom, Christopher Patty, Emma Camarena, Thomas Gray, Regina Sawyer, Brian Brown, Raymie McFarland
BACKGROUND
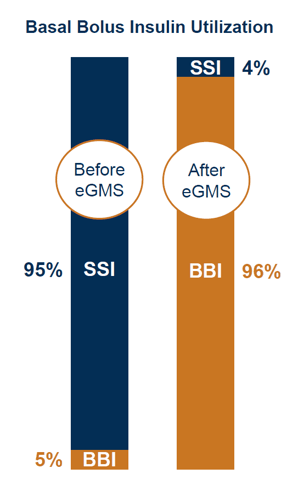
Hyperglycemia affects up to 40% of hospitalized patients and is associated with poor outcomes, including increased mortality, length of stay and surgical site infections. The standard of care is intravenous (IV) insulin therapy for critically ill patients and subcutaneous (SubQ) basal bolus insulin therapy (BBI) for non-critically ill patients. However, despite best practice guideline recommendations from ADA and other associations for use of BBI, use of sliding scale insulin therapy (SSI) persisted at our medical center because of familiarity, lack of diabetes and endocrinology expertise, and concerns over hypoglycemia. Glytec’s eGlycemic Management System® (eGMS®) was selected to facilitate the conversion from SSI to BBI.
METHODS
This retrospective quality improvement case study compared IV and SubQ insulin ‘usual care’ (UC) to that of the nurse-directed, computer-guided Glucommander (GM) solution, an FDA-cleared insulin dosing decision support module of eGMS that is integrated with our medical center’s electronic health record. The primary objective was to measure (with the support of hospital leadership) the clinical effort required to improve education for clinicians, increase utilization of BBI order sets, analyze inpatient glucometrics, and provide safer insulin management. Comparisons were made between pre-eGMS (baseline) data from calendar year 2015 and post-eGMS data from March 2016 through March 2017. Comparisons were also made between patients treated with UC and patients treated with GM during the first year of eGMS use at our medical center.
| PATIENT DEMOGRAPHICS | UC – Usual Care | GM – Glucommander |
|---|---|---|
| #Patients | 1,039 | 3,200 |
| Age | 61.91 | 63.32 |
| Gender – Male | 47% | 48% |
| Gender – Female | 53% | 52% |
| Height (cm) | 166.47 | 166.14 |
| Weight (kg) | 85.75 | 87.99 |
| BMI | 30.91 | 31.62 |
| LOS | 7.18 | 5.51 |
| A1c | 8.97 | 8.49 |
| GFR | 49.85 | 51.72 |
CLINICAL RESULTS
Upon implementing eGMS, our medical center converted to near-exclusive utilization of BBI in our inpatient population. First year results with the computer-guided Glucommander (GM) solution for BBI are as follows.
- Hypoglycemia <70 mg/dL: 2,434 fewer events with GM BBI vs UC SSI
- Hyperglycemia >180 mg/dL: 40,589 fewer events with GM BBI vs UC SSI
- Number of Days on Basal Bolus Insulin Therapy: 4.39 days (80% of total days)
- Number of Total Insulin Dose Adjustments: 69,256
- Number of Basal Insulin Dose Adjustments: 0.84 per day (11,800 total)
- Number of Bolus Insulin Dose Adjustments: 2.02 per day (28,377 total)
- Number of Correction Dose Adjustments: 2.07 per day (29,079 total)
- Number of Dose Recommendations Edited by Prescriber: 0 breakfast, 8 lunch, 7 dinner, 35 basal (50 total); 99.9% not edited
- Number of Dose Recommendations Not Administered by Nurse: 737 total; 98.9% administered as recommended
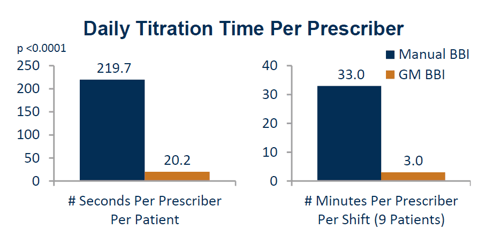
- Daily Titration Time Per Prescriber/Per Patient: 20.2 seconds with GM BBI vs 219.7 seconds (sd +/- 76) with manual BBI
- Daily Titration Time Per Prescriber/Per Shift (9 Patients): 3.0 minutes with GM BBI vs 33.0 minutes with manual BBI
FINANCIAL RESULTS
Use of eGMS in our medical center resulted in substantial reductions in the number of hypoglycemic events and the average length of stay, which contributed to total first year savings of $9,720,556.
| Hypoglycemic Event Savings | $7,141,356 |
|---|---|
| Length of Stay Savings | $2,579,200 |
| TOTAL Annualized Savings | $9,720,556 |
- Reduction in Hypoglycemic Events: 2,434 fewer hypoglycemic events with GM versus UC, resulting in savings of $7,141,356 over the first year.
- Reduction in Average Length of Stay: 1.67 fewer days, resulting in savings over the first year of $2,579,200.
CLINICAL WORKFLOW IMPACT
Use of eGMS in our medical center, and the computer-guided decision support provided by Glucommander (GM), resulted in a reduction of 69,256 insulin dose adjustments (over the first year) otherwise required by prescribers when manually titrating daily basal bolus insulin.
| Time Saved Per Prescriber Per Patient | 199.5 Seconds |
|---|---|
| Time Saved Per Prescriber Per Shift | 30 Minutes |
CONCLUSION
Glycemic management vastly improved with use of eGMS in our medical center. The conversion from SSI to BBI supported by GM enhanced overall patient safety and eliminated the time and effort otherwise required when manually titrating insulin. By reducing hypoglycemia and length of stay with eGMS, we realized a first year savings of $9,720,556.