Glytec eGlycemic Management System in Combination With Clinical Surveillance Reduces Hypoglycemia and Can Identify Patients at Risk of Increased Length of Stay in Hospitalized Patients With Diabetic Ketoacidosis
Presentation
American Association of Clinical Endocrinologists Scientific & Clinical Congress
Date
May 2014
Authors
Joseph Aloi,1 Anthony Williams,2 Robby Booth,3 Harry Hebblewhite,3 Raymie McFarland,3 Bruce Bode4
Objective
Improving the quality and concomitantly decreasing the costs associated with the care of persons with diabetes is a current focus of many healthcare systems. Additionally, there is a renewed interest in care pathways that reduce length of stay while reducing preventable readmissions to the hospital. This study was designed to safely improve the care pathway associated with the management of diabetic ketoacidosis (DKA). This study retrospectively analyzed patient records to evaluate the glycemic outcomes of patients with DKA being treated with Glucommander (GM), an IV insulin infusion dosing tool, versus an insulin protocol.
Methods
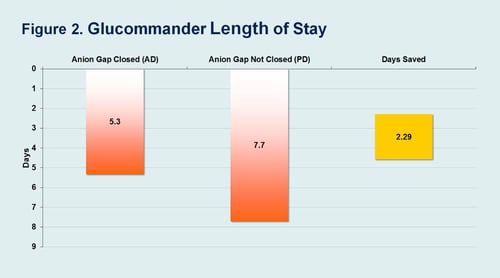
We reviewed the patient medical records of 186 patients with a diagnosis of DKA at 3 community hospitals. The data was collected over a 3-month time period. Qualifying patients had a diagnosis code of DKA (ICD 150.10-250.13), elevated admission glucose (>250 mg/dl), elevated Anion Gap (AG >12 mEq/L), and were treated with GM. A beta model of GlucoSurveillance was applied to the patient records of those patients treated with GM to identify any patient that had uncontrolled glucose (>180 mg/dl) and elevated AG (>12 mEq/L). Treated patients were divided into 2 groups: 116 patients were Appropriately Discontinued (AD) from GM once their AG was within normal limits ( 12 mEq/L). The LOS for each patient was recorded. There was no significant difference in the two study groups with respect to hemoglobin A1c, age, BMI, admission glucose or AG. GM glycemic outcomes, including average initial and day of discharge blood glucose, and hypoglycemia, were also compared to 139 Non-GM DKA patients in the same hospital units.
Results
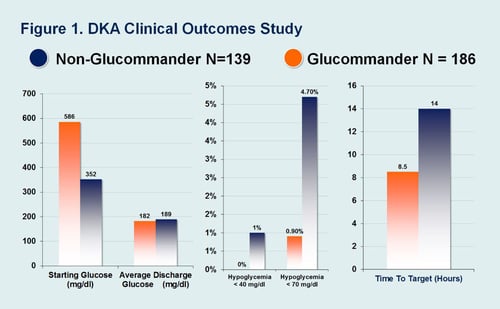
There was no significant difference in glucose at discharge between the two GM groups: PD group (187 mg/dl +/- 83) and AD group (178 mg/dl +/- 69). 100% of patients in both GM groups achieved target glucose. Hypoglycemia was low in both groups, but there was however, an increase in Hypoglycemia when GM was discontinued, with GM patients (0.1%) <40 mg/dl compared with (0.9%) <40 mg/dl for Post GM care. Length of treatment on GM was similar in both Anion Groups at 1.4 days. Length of stay was reduced by 2.29 days with PD patients at 5.33 LOS compared to PMD patients at 7.7 LOS. In the comparison group GM had a lower incidence of hypoglycemia 0.9% vs 4.7% <70 mg/dl (P <0.03). Both GM and Non-GM achieved target glucose levels but the GM group started with a higher BG on IV initiation of 586 mg/dl vs 352 mg/dl, a difference of 234 mg/dl.
Conclusion
This study shows the clinical impact of using the tools available in the eGlycemic Management System, such as Glucommander and GlucoSurveillance, to improve the efficacy, safety and efficiency of care provided to DKA patients in the hospital. Glucommander improved patient safety by reducing the incidence of hypoglycemia in patients with DKA, while bringing 100% of these patients into the glycemic target. Length of Stay was 2 days less for patients treated with Glucommander and appropriately discontinued.
Affiliations
- Eastern Virginia Medical School, Norfolk, Virginia.
- West Tennessee Healthcare, Jackson, Tennessee.
- Glytec, Greenville, South Carolina.
- Piedmont Hospital, Atlanta, Georgia.