Length of stay (LOS) is one of the most important performance indicators for hospitals. Average LOS reflects the quality and efficiency of the care patients are receiving, and strongly correlates with cost of care.
Reducing length of stay can produce direct and meaningful benefits for hospitals, including freed up beds, reduced costs and reduced risk of hospital-acquired infections.
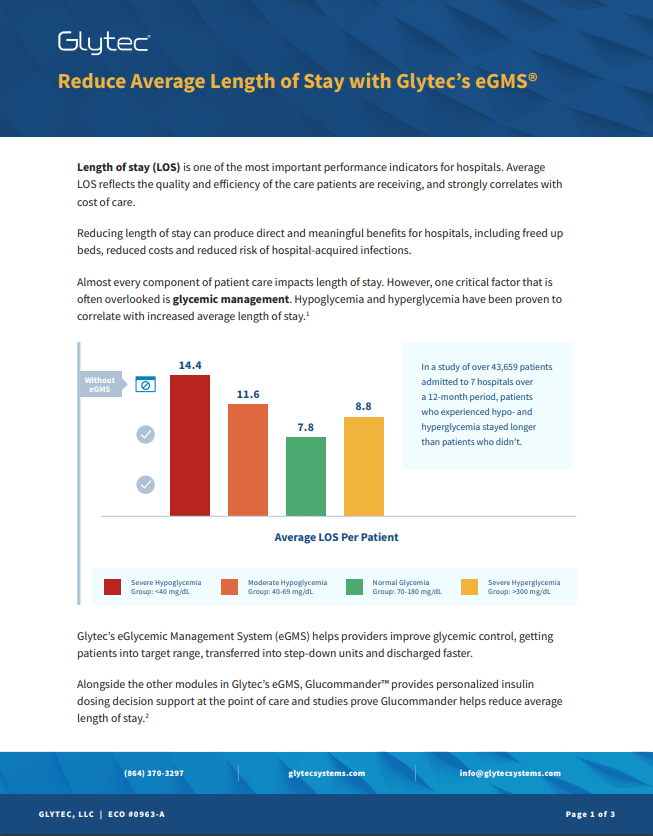
In a study of over 43,659 patients admitted to 7 hospitals over a 12-month period, patients who experienced hypo- and hyperglycemia stayed longer than patients who didn’t.
Glytec’s eGlycemic Management System (eGMS) helps providers improve glycemic control, getting patients into target range, transferred into step-down units and discharged faster.
Alongside the other modules in Glytec’s eGMS, Glucommander™ provides personalized insulin dosing decision support at the point of care and studies prove Glucommander helps reduce average length of stay.2
How eGMS reduces average length of stay
For patients requiring insulin, tightly controlling blood glucose is key to reducing length of stay. Glytec’s eGMS is a comprehensive solution comprised of several modules that help providers control blood glucose.
Glucommander uses an FDA-cleared algorithm to provide personalized insulin dosing recommendations based on standard-of-care methodologies for both IV and SubQ insulin. This EMR-integrated workflow replaces sliding scale and paper protocols, reducing the risk of errors and improving patient outcomes.
eGMS also includes modules that automatically alert staff to patients at risk of hypo- and hyperglycemia, improve the timeliness of blood glucose checks, improve communication within care teams and generate automated glucometrics dashboards and reports.
Using these tools, hospitals using eGMS have been able to:
- Get patients into target blood glucose range faster.3
- Reduce the incidence of both hyperglycemia and hypoglycemia.4
- Guide the transition from IV insulin to SubQ insulin as patients are transferred into step-down units, reducing bounce-back cases.5
Evidence of reduced length of stay using eGMS
At Kaweah Delta Medical Center in Visalia, CA, use of eGMS was shown to reduce average length of stay among patients requiring insulin by 3.18 days compared to usual care.
Beyond length of stay
Reducing average length of stay is just one way Glytec’s eGMS improves quality of care and reduces costs for hospitals. eGMS has also been proven to:

References:
- Financial Implications of Poor Glycemic Management & Improvement Strategies for Optimal Outcomes. IHI Annual National Forum on Quality Improvement in Health Care, Dec 2018.
- Newsom R, Patty C, Camarena E, et al. Safely Converting an Entire Academic Medical Center From Sliding Scale to Basal Bolus Insulin via Implementation of the eGlycemic Management System. J Diabetes Sci Technol. 2018;12(1):53-59. https://journals.sagepub.com/ doi/10.1177/1932296817747619
- Comparative Effectiveness of a Computerized Algorithm Versus a Physician Instituted Protocol to Manage Insulin Infusions After Cardiac Surgery. HMO Research Network Conference, Apr 2014.
- Comparison of Hyperglycemia Management Protocols in the ICU: Standard Protocol versus eGlycemic Management System. American Diabetes Association Scientific Sessions, Jun 2019.
- Carr L., Rogers C., Ryan D., McFarland R., Bernardi N.,Frey K., Haines T. Evaluating the Impact of eGMS- Glucommander on Length of Stay, Hypoglycemia, and Glucose Control Used in a Regional Medical Center. 2018 Diabetes Technology Meeting. 2018. https://glytecsystems.com/ evidence/evaluating-the-impact-of-egms-glucommander-on-length-of-stay-hypoglycemia-and-glucose-control-in-a-regional-medical-center/
- Relationship Between Glycemic Control Using eGMS and Readmission Rates in Cardiovascular Patients Hospitalized with AMI, CHF or Undergoing CABG During the Implementation of a System Wide Glycemic Initiative. Annual Diabetes Technology Meeting, Nov 2016
- New Interfaces for eGlycemic Management System Save Nursing Time and Improve Patient Outcomes: Time and Motion Nursing Study. American Association of Clinical Endocrinologists Scientific & Clinical Congress, May 2014.
ECO #0963-A


.webp?width=650&height=100&name=Sentara-Healthcare_CTA%20(1).webp)