Utilization of Computer-Guided Insulin Dosing Reduces Hypoglycemia Adverse Drug Events, Length of Stay and Hospitalization Costs at a Large Pacific Northwest Health System
Presentation
Diabetes Technology Society (DTS) Virtual Poster Meeting
Date
June 18, 2020
Authors
Jamie Casanova, PharmD, BCPS, Ann Ohlin, ARNP, Dan Yamasaki, MA, MS, MBA
OBJECTIVE
Determine whether use of the eGlycemic Management System® (eGMS®)*, an EHR-integrated software platform for intravenous and subcutaneous insulin dosing in the acute care setting, results in improved clinical and financial outcomes among hospitalized patients.
*eGlycemic Management System® is a registered trademark of Glytec, LLC on behalf of Aseko, Inc. All Rights Reserved.
METHOD
CHI Franciscan (CHIF), an 8-hospital, 1,200-bed health system in Washington State, struggled with adoption of basal-bolus insulin despite development of standardized insulin order sets and staff education initiatives. As a participant in Washington State Hospital Association’s Adverse Drug Event Quality Initiative for glycemic control, rates of hypoglycemia at CHIF were shown to be higher than other hospitals in the state.
In January 2018, CHIF implemented eGMS® for prescriber-directed insulin dosing. In preparation, the CHIF Glucose Steering Committee coordinated:
- Revision and optimization of insulin order sets
- Education and training for nurses, providers and pharmacists
- Augmentation of pharmacist role to identify patients for eGMS® insulin titration
- Data collection to support glycemic outcome metrics
- Monthly data and process reviews by the Glucose Steering Committee
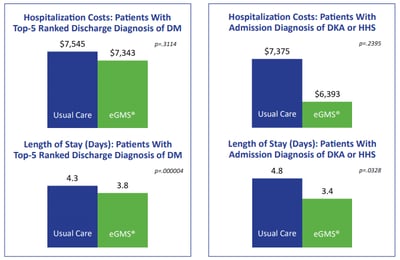
An initial retrospective analysis examined length of stay and hospitalization costs among patients with a top-5 ranked discharge diagnosis of diabetes (DM) and those with an admission diagnosis of diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS). This analysis compared patients treated using standard protocols, i.e., a non-eGMS® usual care control group (September 2017 through April 2018) to patients treated using eGMS® (January 2018 through April 2018).
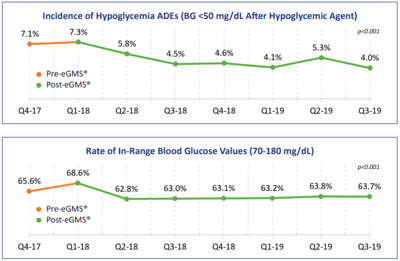
A subsequent retrospective analysis compared incidence of hypoglycemia ADEs (defined as a blood glucose value <50 mg/dL following administration of a hypoglycemic agent) and rate of in-range blood glucose values 70-180 mg/dL before eGMS® implementation (September 2017 through December 2017) to after eGMS® implementation (January 2018 through December 2019).
RESULT
When comparing eGMS® to standard protocols (usual care), length of stay was 0.5 days less and hospitalization costs were $202 less among patients with a top-five ranked discharge diagnosis of DM; likewise, length of stay was 1.4 days less and hospitalizations costs were $982 less among patients with an admission diagnosis of DKA or HHS.
Incidence of hypoglycemia ADEs declined from an average of 7.1% in the quarter before eGMS® implementation to an average of 4.0% after eGMS® implementation (in the most recently-reported quarter), for a overall reduction of 43.7% (p<0.001).
Rate of in-range blood glucose values declined from an average of 65.6% in the quarter before eGMS® implementation to an average of 63.7% after eGMS® implementation (in the most recently-reported quarter), for a overall reduction of 1.9% (p<0.001).
CONCLUSIONS
A comparison of pre-intervention data (April 1, 2016 – March 31, 2017) to post-intervention data (April 1, 2018 – March 31, 2019) revealed we reduced all-cause critical hypoglycemia <40 mg/dL by 16.9% of patient days (from 0.65% to 0.54%). The most significant improvements were associated with four areas of targeted interventions: (1) failure to follow policy, (2) stacking insulin, (3) wrong insulin dose, and (4) failure to adjust insulin. We attribute our success to clinical practice changes and quality improvement initiatives coupled with the implementation of a technology-enabled approach to intravenous infusion and subcutaneous basal-bolus insulin dosing using an eGlycemic Management System®.
We recommend that any hospital seeking to achieve best practice and clinical excellence in glycemic management perform a similar root cause analysis of critical hypoglycemic events, define the most appropriate targeted interventions, and utilize education, accountability, workflow and policy measures to achieve their goals.
References
- Casanova J, Ohlin A, Yamasaki D. Utilization of Computer-Guided Insulin Dosing Reduces Hypoglycemia Adverse Drug Events, Length of Stay and Costs at a Large Pacific Northwest Health System. DTS Virtual Poster Meeting. June 18, 2020.
ECO #0847-A