Presentation
International Conference on Intensive Insulin Therapy for Tight Glycemic Control
Date
June 2007
Authors
Bruce Bode
KEY POINTS
- Hospital protocols to control glucose must be simple and user-friendly.
- These protocols should allow patients with hyperglycemia to be treated the same, allowing modification and refinement of the protocol only when necessary.
- There are two effective methods for normalizing glucose for hospitalized patients: continuous, variable-rate intravenous (IV) insulin infusions and basal bolus subcutaneous (SC) insulin therapy.
- Computerized algorithms for IV insulin infusion and transition to SC insulin therapy enable standardization that can minimize medical errors made in insulin dosing.
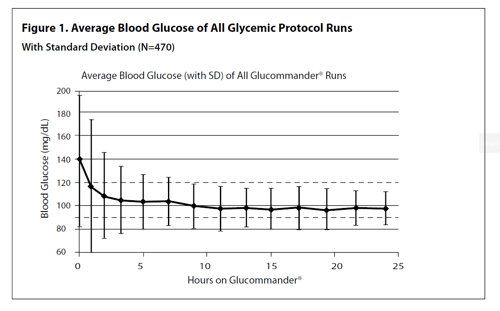
- The use of a computerized protocol for cardiovascular surgery patients resulted in near-normal glycemia (mean blood glucose 107 mg/dL) with no blood glucose <40 mg/dL.
INTRODUCTION
Studies have shown the benefits and risks of tight glycemic control (TGC) in hospitalized patients, including the intensive care unit (ICU).1-4 TGC methodologies can be difficult to implement because they often require complex, insulin-dosing formulas that are restricted to the ICU, and highly skilled nurses to work with only one or two patients at a time. Severe hypoglycemia also can be a problem with many intravenous (IV) insulin protocols and has been shown to be an independent risk factor for mortality.5 In this article, the methodology, results and benefits of a computerized protocol in cardiovascular (CV) patients undergoing bypass or valve surgery are discussed.
The recommended goals for glycemic control in the hospital vary slightly between the American Association of Clinical Endocrinologist (AACE) and the American Diabetes Association (ADA). Both organizations recommend a blood glucose level <110 mg/dL in the ICU. AACE recommends <110 mg/dL premeal with peak postprandial <180 mg/dL, while the ADA recommends 90-130 mg/dL premeal.6
To accomplish these goals while minimizing the risk of hypoglycemia, protocols can be developed and implemented to screen patients at high risk for hyperglycemia and to modify and initiate insulin therapy when needed. If a patient is acutely ill or unable to eat, a continuous, variable-rate IV insulin infusion based on hourly or more frequent glucose measurements should be used. If a patient is stable and able to eat, subcutaneous (SQ) basal bolus therapy can be used, with blood glucose measured premeal, at bedtime and at 0300. Transition from IV to SC basal bolus insulin therapy should be done with known or newly diagnosed patients with diabetes who had pre-existing glycemia based on an A1c >6%. Discharge planning should be done for all patients with diabetes who have not received insulin before, including those who are newly diagnosed. Case-specific recommendations are made for diabetes management at home.
METHODOLOGY
Based on the above goals, Piedmont Hospital in Atlanta decided to implement a TGC protocol in CV patients undergoing bypass and valve surgery. This decision was made after analysis of data from the preceding six months that revealed that only 50% to 60% of CV patients had met the Institute for Healthcare Improvemement’s goal of having all blood glucose levels be <200 mg/dL in the 24 hours post-surgery.7 To achieve this goal, a team of endocrinologists, nurses, pharmacists and educators met with a CV surgeon every week for three months to develop the protocol. All parties agreed to the following:
- The protocol would be used for all patients, so that all patients would be treated the same.
- Since CV patients are at high risk for hyperglycemia, upon arrival at the hospital all patients would be screened for both A1c and glucose.
- If a patient were admitted >24 hours before surgery, a weight-based basal bolus SQ insulin would be initiated if the A1c were >6% or the premeal blood glucose was >140 mg/dL. The weight-based formula used in the protocol is weight in Kg times 0.5 equals total daily dose (Kg x 0.5 = TDD), with 50% of the basal being given as glargine insulin at bedtime and the remaining 50% of insulin divided by 3 and given as a pre-meal dose of rapidacting insulin (RAI). Bedside capillary blood glucose would be measured premeal, at bedtime and 0300, with a correction dose of RAI given for a blood glucose >140 mg/dL. The correction formula would be blood glucose minus 100, divided by correction factor as determined by the 1700 rule, which is 1700 divided by the TDD ([blood glucose – 100] / [1700/TDD]).
- Within the the 24-hour period pre-surgery through the peri-operative period, computerized IV insulin delivery using Glucommander would be initiated for anyone with one blood glucose >140 mg/dL or two blood glucose >110 mg/dL8. Targets for glucose control would be 90-120 mg/dL with blood glucose measurement in response to a Glucommander alert (average, hourly; range, every 20 to 120 minutes based on the stability of the glucose). The lower alert target of 90 mg/dL was selected to minimize the risk of hypoglycemia. Maintenance intravenous fluids (IVFs) are administered using D10W at 50mL/hr to prevent catabolism and allow a 1-to-1 conversion of IV units to SC units.
- Hypoglycemia (<60 mg/dL) would be treated with 50% Dextrose IV, based on the following formula: (100 – blood glucose) x 0.4 = mL of D50 IV push.
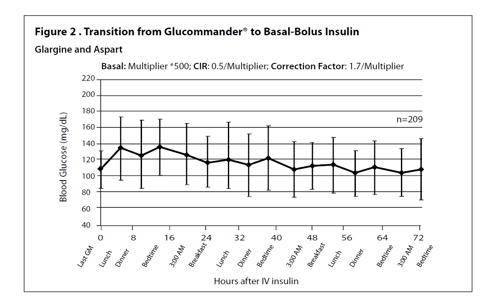
- IV insulin therapy would be continued until the morning of postoperative day (POD) #2 and longer if a patient were unable to eat or still critically ill. Transition to SC basal bolus therapy would be done only if the patient had known diabetes or an A1c >6%. The transition is initiated by giving glargine insulin at 11p.m. POD #1 if the patient is stable, with RAI given premeal the following morning and stopping of the IV insulin and IVFs post-breakfast. The TDD was calculated by using the multiplier on the Glucommander at 11 p.m. the night of transition, with the glargine dose being 500 times the multiplier, the RAI dose being the same dose divided by 3 and given in proportion to the food consumed, and the correction dose given as listed in the weight-based formula. Insulin SQ doses would be adjusted by 20% if blood glucose readings were outside the 70-140 mg/dL range. Diet therapy would be initially 1800K cal ADA diet in all patients with adjustment based on nutrition consultation.
- Discharge planning and diabetes education would be provided for all patients who have not self-administered SQ insulin and patients with a change in their insulin regimen. All patients with A1c >7% would be instructed to remain on their basal bolus insulin therapy for at least 4 to 6 weeks or longer, until advised otherwise by their primary care practitioner.
- An endocrinologist would be consulted for any patient with a blood glucose <70 or >140 mg/dL or a patient who had not received insulin before.
RESULTS
The above protocol was initiated in January 2006 with a one-month pilot followed by use for all patients in February 2006. As of October 2006, more than 1,800 patients have been treated using this protocol. Data from the first 470 patients were analyzed, producing the following results.
- 28% of patients had pre-existing diabetes with 10% of all patients being on insulin pre-admission; 48% of patients had an A1c >6% with 52% having one or more of these three criteria.
- 96% of patients needed IV insulin peri and post-operatively with the time to <120 mg/dL being 3 hours. IV insulin was continued for a mean of 37 hours. Mean blood glucose was 107 mg/dL with 2% of patients having a transient blood glucose <50 mg/dL and no patient having a blood glucose <40 mg/dL (Figure 1).
- 98% of patients have been controlled with no blood glucose >200 mg/dL within the first 48 hours postoperatively.
- 55% of patients were transitioned to basal bolus therapy whereby >90% of the blood glucose values remained in the target range (70-140 mg/dL) with no blood glucose <40 mg/dL (Figure2).
- 23% of patients were discharged with home insulin therapy: >90% of those were discharged on basal-bolus therapy.
- Nursing feedback after the first 60 days was uniformly positive: the only major initial complaint was the frequency of glucose monitoring while a patient is on IV insulin. Complaints subsided after nurses realized that patients had fewer infections and shorter length of stay. Agency and float nurses were able to learn the protocol within their first shift on the CV ICU postoperative unit or CV floor.
- Physician acceptance of the protocol has been uniformly positive with no criticisms or complaints.
- Post-operative length of stay was reduced by 0.8 days for an estimated annual savings of over >$800,000
CONCLUSIONS
This glycemic protocol using a computerized system for IV insulin infusion and transition to SC basal bolus insulin therapy was highly effective in normalizing blood glucose without significant hypoglycemia in all patients undergoing CV surgery at Piedmont Hospital in Atlanta. Several important factors were involved in achieving this success. The protocol was designed and implemented as a group effort by diabetes specialists, nurses, pharmacists and educators under the guidance of a CV surgeon who championed the program to his fellow surgeons and hospital administration. Empowerment of the nurses in the design, ownership and implementation of the protocol was crucial. Use of a proven, computerized, IV-insulin-dosing algorithm (Glucommander) with appropriate setting of the target range of 90-120 mg/dL allowed all patients to obtain a mean glucose of 107 mg/dL with no glucose <40 mg/dL.
Transition from IV to SQ insulin in all patients with known diabetes or an A1c >6% allowed normalization of blood glucose after eating during the post-operative period until discharge. To accomplish this, all patients were screened for diabetes and had an A1c drawn to identify patients to transition from IV to SQ insulin and who would benefit from insulin after discharge. Any patients admitted with poorly controlled diabetes were normalized in the hospital with insulin and discharged with an insulin regimen to keep their blood glucose levels normal as long as they complied with their case-specific regimen. It is felt by all team members that such a glycemic protocol could also be used in normalizing glucose in other patients in the hospital system.
REFERENCES
- Van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in the critically ill patients. N Engl J Med 2001; 345:1359-67. 2001.
- Furnary AP, Gao G, Grunkemeier GL, et al. Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003 May;125(5):1007-21.
- Krinsley JS. Effect of intensive glucose management on the mortality of critically ill adult patients. Mayo Clin Proc. 2004;79:992-1000.
- Gandhi GY, Nutta GA, Abel MD, et al. Intensive intraoperative insulin therapy versus conventional glucose management during cardiac surgery, a randomized trial. Ann Intern Med 2007;146:233-43.
- Krinsley JS, Grover A. Severe hypoglycemia in critically ill patients: risk factors and outcomes. Crit Care Med. 2007 Oct;35(10):2262-7.
- American College of Endocrinology and American Diabetes Association Consensus Statement on In-Patient Diabetes and Glycemic Control. Endocr Pract. 2006 Jul-Aug 12(14):458-68 and Diabetes Care 2006 Aug 29; (8):1955-62.
- Institute for Healthcare Improvement website: Institute for Healthcare Improvement website: www.IHI.org/IHI/Topics/PatientSafety/SurgicalSiteInfections/Changes/SSI+Maintain+Glucose+Control.htm