Presentation
Annual Wireless Health Conference
Date
October 2014
Authors
Stephen Ingram, Laurel Fuqua, Robby Booth, Andrew Rhinehart, Randall Ball, Tamera Parsons, Raymie McFarland
Introduction
Prevention of hypoglycemia and hyperglycemia are important for the proper management of diabetes as these acute complications are not only costly to a health system but are of particular concern to patients who are living daily with diabetes. In addition, many patients with diabetes have multiple chronic conditions, some of which are behavioral health conditions. Management of diabetes in psychiatric/behavioral health patients can be even more challenging, given the associated behaviors of some mental illnesses and their treatment with psychotropic drugs. This is particularly an issue for patients using insulin. Both patients and their health care providers often struggle to find the appropriate insulin dose for metabolic control in acute care, ambulatory care such psychiatric facilities and in outpatient settings. Today, however, new, innovative wireless and cloud based technology is helping to address this important problem regardless of the health care setting. The wireless and cloud based capabilities allow solutions to be deployed across the entire care continuum. This poster represents the results of the use of an innovative cloud based technology to dose insulin that decreases the acute complications of diabetes regardless of health care setting.
Purpose
Mountain States Health Alliance (MSHA), a healthcare system with 13 hospitals, serving 29 counties in Tennessee, Virginia, Kentucky, and North Carolina, has achieved substantial decreases in the incidence of hypoglycemia and hyperglycemia in ICU and acute care inpatients by using Glytec’s e-Glycemic Management System. Included in MSHA’s integrated healthcare delivery system is Woodridge Hospital, an 84-bed inpatient provider of mental health and chemical dependency services for adults, adolescents, and children ages 6 and older.
The medical staff at Woodridge Hospital historically experienced challenges in managing diabetes within a mental health institution due to the population characteristics, concomitant medications, medication delivery system, food delivery and access issues. Many of their ambulatory patients have diabetes and some had been transferred to acute care hospitals or ERs to treat severe hypoglycemia. As a result, the organization deployed the eGlycemic Management System to achieve lower rates of hypoglycemia in a high-risk, ambulatory, inpatient population.
Methods
In early 2014, the Team planned a glycemic improvement project for the hospital, which included the deployment of Glytec’s eGlycemic Management System, a cloud-based system that provides IV and SubQ insulin dose calculations for adult and pediatric patients. Nurses and physicians were trained on the use and starting in April 2014, patients needing insulin who met criteria were placed on the system.
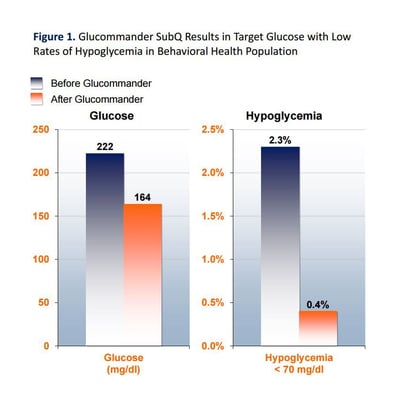
Before the project started, baseline glucose rates 200 mg/dl+ and 2.3% of all blood glucose readings indicated Hypoglycemia (blood glucose <70 mg/dl).
In July 2014, the team conducted a retrospective chart audit of all 83 patients who had been placed on the System to determine the impact on hyper/hypoglycemia. Metrics to be collected were: (1) average starting glucose before Glucommander, (2) average glucoses on Glucommander SubQ, (3) % reduction of glucose averages, and (4) % of hypoglycemia events by point of care reading <70 mg/dl.
Results
83 patient charts were reviewed and a total of 1,513 total BGs were analyzed. Glucommander treated patients showed a 26% improvement in glycemic control from a starting glucose of 222 mg/dl to a fasting glucose of 164 mg/dl. Hypoglycemia was very low with a 0.40% less than 70 mg/dl (baseline hypoglycemia at WPH before Glucommander implementation was 2.3% <70 mg/dl).
Results seem to indicate that a cloud based, wireless eGlycemic management solution can be deployed to assist health care providers with managing glycemic control in patients across the entire care continuum and with complex populations. The system was deployed in acute care settings within a hospital system and then also deployed and used with ambulatory psychiatric patients. The results with 83 ambulatory patients showed a 26% improvement in glycemic control and an extremely low incidence of hypoglycemia. Decreasing the acute complications of diabetes also correlates with decreased ER visits and hospital admissions.
The ability to successfully achieve quality and cost outcomes with the use of wireless, cloud based technology to address insulin management in complex populations has implications for today’s new and emerging health care models. Technology solutions that can be deployed across an entire care continuum and with divergent populations can contribute to solving the cost/quality equation for all stakeholders. These results indicate that a standardized approach coupled with the use of innovative technology and can help directly improve the overall health and safety of an ambulatory high risk population of patients who have diabetes. Further studies in other settings and with other diabetes populations is indicated.