Presentation
American Association of Clinical Endocrinologists Scientific & Clinical Congress
Date
May 2016
Authors
Joseph Aloi,1 Paul Chidester,2 Amy Henderson,3 Robby Booth,3 Raymie McFarland,3 April Mumford,4 Jagdeesh Ullal5
Background
Hypoglycemia is a common adverse event for patients treated with insulin in the hospital setting, and is often considered the rate-limiting step for optimizing inpatient glycemic management. Fear of hypoglycemia commonly leads clinicians to deviate from best practice recommendations such as the use of scheduled basal/bolus therapy (BBT) for non-critically ill patients as recommended in the 2009 AACE and ADA Consensus Statement. For critically ill patients hypoglycemia is thought to be a biomarker of the severity of disease; however, some percentage of these events are hypothesized to be preventable. Known risk factors for hypoglycemia include: treatment with insulin, previous hypoglycemic events, poor nutritional intake, renal insufficiency or failure, limitations of intravenous (IV) paper protocols and missed opportunities to titrate subcutaneous (SubQ) insulin to goal.
Methods
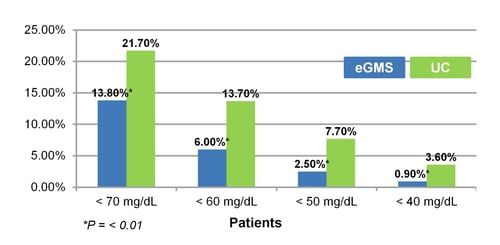
The aim of this study is to compare hypoglycemia rates for patients managed on an Electronic Glycemic Management System (eGMS) vs. patients managed by Usual Care (UC). There were 13,351 patients treated with eGMS and 45,335 patients treated with UC. The target blood glucose (BG) was set at 100-180 mg/dL. This study evaluated the percent of patients experiencing mild to moderate hypoglycemia (<70, <60, <50 mg/dL) and severe hypoglycemia (<40 mg/dL) on eGMS vs. UC. Admission blood glucose and mean blood glucose were also measured for both groups.
| Patient Characteristics | eGMS | UC |
|---|---|---|
| Number of Patients | 13,351 | 45,335 |
| Average BG | 178 mg/dL | 188 mg/dL |
Results
- The incidence of patients experiencing any hypoglycemia <70 mg/dL was 13.8% for eGMS compared to UC at 21.7% (P = <0.01).
- The GMS had 6% <60 mg/dL and 2.5% <50 mg/dL compared to UC at 13.7% (P = <0.01) and 7.7% (P = <0.01).
- The eGMS also had less severe hypoglycemia at 0.9% of patients with a BG <40 mg/dL compared to UC at 3.6% (P = <0.01).
- The average BG for patients treated on eGMS was 178 mg/dL compared to UC at 188 mg/dL.
Conclusion
The eGMS had a lower number of patients with hypoglycemia and lower average BG during hospitalization compared to UC, suggesting it may be easier to achieve glycemic targets safely using best practice methodologies such as BBT for patients in the hospital setting. This may be accomplished through utilization of features that target known risk factors for hypoglycemia and titrate insulin to goal using a prescribed target range. Benefits of eGMS IV and SubQ insulin algorithms include patient-specific insulin dosing that calculates a patient’s insulin sensitivity and SubQ algorithms that have additional benefits of matching insulin to carbohydrate intake for patients with poor nutritional intake or NPO during hospitalization. More prospective studies are needed to assess improved hypoglycemia rates of eGMS vs. UC.
Affiliations
- Wake Forest Medical Center, Winston Salem, North Carolina.
- Sentara Healthcare, Norfolk, Virginia.
- Glytec, Waltham, Massachusetts.
- Mountain States Health Alliance, Johnson City, Tennessee.
- Eastern Virginia Medical School, Norfolk, Virginia.