Financial Implications of Glycemic Control: Results of an Inpatient Diabetes Management Program
Publication
Endocrine Practice
Date
August 2006
Authors
Christopher Newton,1 Sandra Young2
Abstract
Objectives: (1) To determine the financial implications associated with changes in clinical outcomes resulting from implementation of an inpatient diabetes management program and (2) To describe the strategies involved in the formation of this program.
Methods: The various factors that influence financial outcomes are examined, and previous and current outcomes are compared.
Results: Associations exist between hyperglycemia, length of stay, and hospital costs. Implementation of an inpatient diabetes management program, based on published guidelines, has been shown to increase the use of scheduled medications to treat hyperglycemia and increase the frequency of physician intervention for glucose readings outside desired ranges. Results from implementing this program have included a reduction in the average glucose level in the medical intensive care unit through use of protocols driven to initiate intravenous insulin once the glucose level exceeds 140 mg/dL. Additionally, glucose levels have been reduced throughout the hospital, primarily because of interactions between diabetes nurse care managers and the primary care team. Associated with these lower glucose levels are a decreased prevalence of central line infections and shorter lengths of stay. The reduction in the length of stay for patients with diabetes has resulted in a savings of more than $2 million for the year and has yielded a 467% return on investment for the hospital.
Conclusion: Improved blood glucose control during the hospitalization of patients with known hyperglycemia is associated with reduced morbidity, reduced hospital length of stay, and cost savings. The implementation of an inpatient diabetes management program can provide better glycemic control, thereby improving outcomes for hyperglycemic patients while saving the hospital money.
Associations Between Glycemic Control, Length of Stay, and Cost
Patients with diabetes are known to require longer lengths of hospitalization for any given admission diagnosis (1-4). This increased stay is most likely related to the degree of hyperglycemia present during the course of hospitalization. Estrada et al (5) found that the length of stay (LOS) among cardiac surgery patients with diabetes was 0.76 days longer for every 50-mg/dL increase in glucose. Similarly, hyperglycemia has been found to be an independent predictor of LOS among trauma patients (6).
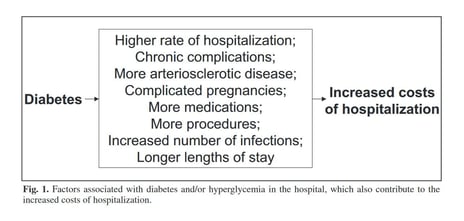
Longer LOS in the hospital may be expected to increase the hospitalization costs. The 0.76-day increased LOS in the cardiac surgery population is associated with a cost increase of $2,824 (5). Although the increased cost of hospitalization for patients with diabetes can be related to LOS, other factors also may contribute to this cost (4). Several of these are illustrated in Figure 1. It should be noted that, although each factor listed can independently increase the costs incurred, there is significant overlap between the factors themselves. For example, the higher rates of infection will prompt increased antibiotic use (thus, more medications) and longer LOS.
Several recent studies have demonstrated that lowering the average blood glucose level of hospitalized patients has significant beneficial effects on important clinical outcomes, such as mortality and infection rates (7-9). Because many of the factors related to increased cost are influenced by the degree of hyperglycemia, it might be predicted that efforts to reduce hyperglycemia would at least have an indirect impact on the cost. Furnary et al (9) have found that, among cardiac surgery patients, the implementation of intravenous insulin protocols to deliver intensive glycemic control results in a substantial decrease in deep sternal wound infections with a subsequent decrease in both cost and LOS when compared with historical data. Intensive insulin management protocols in the surgical intensive care unit (ICU) resulted in improved medical outcomes, with a reduction in ICU stay resulting in an estimated yearly cost savings of $40,000 per ICU bed (10).
Unfortunately, most of the benefits resulting from treating patients with hyperglycemia, including reducing hospitalization costs, are based on studies in which patients received treatment in the ICU. Although ICU care certainly is associated with substantial costs, most hospitalized patients do not receive treatment in the ICU. It would be reasonable to expect that a reduction in blood glucose levels in non-ICU patients also would translate into less expense because of fewer hyperglycemic complications (such as infections) and shorter LOS. Levetan et al (11) demonstrated that the use of a diabetes consultation team resulted in a 56% decrease in LOS, with a corresponding cost reduction of $2,353 per patient. Similarly, Koproski et al (12) observed benefits from using a diabetes team for hospitalized patients. Efforts to implement changes in patient care to achieve the glycemic targets set forth in the American Association of Clinical Endocrinologists (AACE) position statement (13) and the American Diabetes Association technical review (14) on inpatient hyperglycemia would be expected to have a positive impact not only on the morbidity and mortality rates associated with hyperglycemia but also on hospitalization costs.
Implementation of an inpatient diabetes management program
The AACE Position Statement on Inpatient Diabetes and Hyperglycemia contains a series of strategies to assist with improving glycemic management (13). These include an assessment of the existing glycemic control methods, formation of a team comprised of key personnel, recognition of the increased insulin requirements of hospitalized patients, standardization of protocols, and discharge planning. The development of an inpatient diabetes management program encompassed these strategies.
An initial step that preceded the development of this inpatient diabetes management program was the review of current practices at the hospital and a general assessment of the scope of the problem. American Healthways, Inc. (Nashville, TN) was contracted to provide the assessment of current practices and a gap analysis, as well as disease-management options. In the initial assessment, Pitt County Memorial Hospital (a 750-bed, tertiary care, level 1 trauma center in Greenville, NC) had reported 29,010 discharges during the year preceding implementation of the program. This initial assessment was used to establish the baseline practice characteristics as well. Of the more than 29,000 discharges, 23% of patients had a listed diagnosis of diabetes. As expected, the prevalence of diabetes varied by service, with 38% of patients on the cardiothoracic surgery service having diabetes as a diagnosis. Although 23% of the discharged patients had diabetes, this group accounted for more than 26% of the hospital-bed utilization, with a hospital LOS 1 to 2 days longer than that of patients without diabetes. Of note, 63% of the patients with diabetes were Medicare beneficiaries.
Following this initial assessment of the burden of diabetes at the hospital, a gap analysis was performed, which identified several areas for potential improvement. These areas highlighted the need for more prompt interventions for hyperglycemia and greater utilization of basal anti-diabetes medications in lieu of the sliding-scale-only approach. Other improvement opportunities included providing optimal treatment of hypoglycemia, teaching basic diabetes survival skills, and giving dietary instructions. The gap analysis indicated that improvements could be made to reduce the differences in LOS between patients with and without diabetes. This latter opportunity, when viewed in the context of potential cost savings for the hospital (i.e., resulting from shorter LOS) helped garner support from hospital administration for the formation of the diabetes management program.
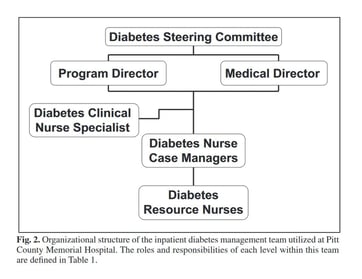
The assessment provided by American Healthways included recommendations for the structure of the diabetes management team, which is illustrated in Figure 2. The roles and responsibilities of the various team members are described in Table 1. From the assessment of disease burden, it was determined that 5 nurse case managers (NCMs) would be needed to provide services to approximately 85% of the patients with diabetes in the hospital. These case managers were assigned to the medical-surgical units that had the highest volume of patients with diabetes. One of their job requirements has been to screen all patients on those units for glucose values below 70 mg/dL or above 140 mg/dL. Whenever a patient who meets these screening requirements is identified, the NCM then seeks to uncover opportunities for improving glycemic management, such as identifying patients for whom sliding-scale insulin orders were written without scheduled diabetes medications being prescribed as well. The case manager will then use daily interactions and collaboration with the residents, attending physicians, and nursing staff to improve the glycemic management.
As noted in Table 1, the Program Director and the Medical Director have been responsible for implementing the policies decided on by the Steering Committee. Evidence-based policies developed by the Steering Committee include protocols for the management of hyperglycemia and hypoglycemia. The diabetes NCMs direct the medical staff toward these protocols during their interactions with medical staff, although the protocols also are available to the staff on units without an assigned diabetes NCM. Moreover, protocols have been developed to assist staff with initiating variable-rate intravenous insulin infusions in the ICU. The cardiothoracic surgery service opted to continue using the intravenous insulin protocol, which had been introduced a year before the start of the inpatient diabetes program, described by Furnary et al (9) for their patients. The Steering Committee decided to use Glucommander (15), a computer software program that assists with the calculation of insulin infusion rates. The software was made available through the consultant’s contract with American Healthways, for the management of the insulin infusions in other critical care areas.
Table 1. Roles and Responsibilities of the Various Members of the Inpatient Diabetes Management Program
| Diabetes Steering Committee |
|
|---|---|
| Program Director |
|
| Medical Director |
|
| Diabetes Clinical Nurse Specialist (CNS) |
|
| Diabetes Nurse Case Managers (NCMs) |
|
| Diabetes Resource Nurses (DRNs) |
|
Clinical impact of a diabetes management program
Several clinical improvements have been observed since implementation of the inpatient diabetes management program. Policy changes in the management of hyperglycemia in the ICU have included initiation of intravenous insulin therapy (targeting a glucose range of 70 to 110 mg/dL) for all nondiabetic patients with glucose readings above 140 mg/dL on 2 occasions, or on 1 occasion for those with known diabetes. Results of these changes have included a reduction in the monthly average glucose values in the medical ICU, from 169.4 ± 66.1 to 123.5 ± 56.1 mg/dL (P <0.0001). Hypoglycemia, defined as a glucose value of <70 mg/dL, has been noted for 7.98% of glucose readings in the medical ICU following the institution of intensive glycemic control, compared with 2.60% of readings in the previous year. The prevalence of severe hypoglycemia, defined as a glucose level of <40 mg/dL, has remained essentially unchanged, with 0.78% of the readings prior to the program and 0.77% following its initiation meeting this definition. A reduction in central line infections also has been observed. Since implementation of these glycemic control measures in the ICUs, the rate of catheter-related bloodstream infection (CR-BSI) has been reduced 33.5% (compared with the rate in the year preceding the program).
Effects of the inpatient diabetes management program are also observed in non-ICU areas. Within the first 6 months of the program being implemented, modifications in behaviors were becoming apparent through random chart audits. Before the program, blood glucose monitoring was performed at least daily for 90.0% of patients with known diabetes; this increased to 98.53% after implementation of the program. Similarly, the proportion of patients for whom a basal dose of an anti-diabetes medication was prescribed (rather than just sliding-scale insulin) increased from 37.5% to 71.7% in the first 6 months. In addition, physicians were noted to be intervening more frequently when 2 or more glucose readings were outside the range of 70 to 200 mg/dL within 24 hours.
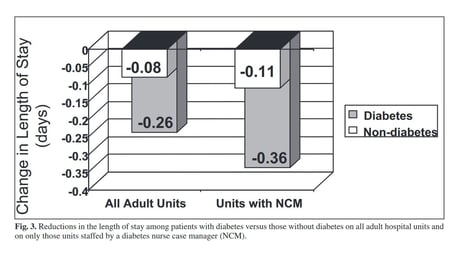
The diabetes management program also has impacted other clinical outcomes. Glucose levels throughout the hospital have been reduced from a monthly average of 177 mg/dL to 151 mg/dL (P <0.0001). Associated with this 26-mg/dL decrease in glucose level has been a reduction in LOS for patients with a diagnosis of diabetes, from 6.01 ± 0.32 to 5.75 ± 0.38 days (P = 0.01). During this same time, no significant change occurred in LOS for patients without diabetes (5.11 ± 0.28 versus 5.03 ± 0.18 days, P = NS). Since the case-mix index for patients with diabetes also increased during this time, it is presumed that the shorter LOS is directly attributable to the reduction in glucose levels.
Additional evidence of the diabetes management program’s impact comes from examining the effects of the NCMs. As shown in Figure 3, the reduction in LOS is even greater for diabetics on units with a NCM assigned to assist with glucose control. This 0.36-day reduced LOS is the major contributor to overall LOS reduction among patients with diabetes in our hospital. Considering that the same physicians manage the patients with diabetes on the hospital units not staffed by diabetes NCMs, and that the same order sets and protocols are available on those units, one possible explanation for the greater reduction in LOS on units with NCMs is the increased attention to glycemic control that results from having a team of nurses who contact the responsible physicians, making them constantly aware of hyperglycemic events and thereby prompting timely intervention to address the elevated glucose levels.
Financial effects of a diabetes management program
Although the implementation of an inpatient diabetes management team has been associated with some significant improvements in clinical outcomes, the cost-effectiveness of these changes also must be evaluated. Tight glycemic control in the medical ICU has reduced the number of CR-BSIs. Central line infection is associated with additional costs, reportedly $3,700 to $56,167 per event (16,17). Thus, it appears that improving glucose control in the ICU, which has reduced the rate of these infections, also would yield a direct cost savings. Even though intravenous insulin therapy is known to incur higher costs in terms of medication expenses compared with subcutaneous insulin regimens, a clear financial benefit of intensive insulin infusion still exists. With one third the number of CR-BSIs, the cost savings for the hospital obviously depends on the initial prevalence of these infections. Using the current Centers for Disease Control (CDC) average central line infection rate of 5 infections per 1,000 catheter use-days (18), the 33.5% reduction in infection rates would save 1.675 infections per 1,000 event days. With the conservative value of a minimal increase in cost of $3,700 per infection, this rate reduction would save $6,197.5 per 1,000 event days. Such savings can be compared with the additional expense of $16.25 per patient per day for intravenous insulin therapy.
As indicated earlier, most patients in the hospital do not receive care in an ICU setting, and thus much of the money spent on patient care occurs in the general medical and surgical care wards. Because of the intrinsic interplay between the multiple reasons for the higher costs of care that occur secondary to hyperglycemia, a challenge exists in accounting for all cost savings secondary to improved glycemic control. Acknowledging that the increased cost of care for patients with diabetes encompasses more than just an increase in LOS, an assessment of the cost benefits of glycemic control in light of its impact on LOS provides insight into the economic impact a diabetes management program can have on a hospital.
The cost savings associated with shorter LOS may be examined in several ways. One viewpoint involves “cost aversion,” which is particularly relevant for patients who have a predetermined reimbursement based on a diagnostic related group. The shorter LOS for these patients means that fewer resources are spent caring for these individuals. Another perspective is to consider the increased bed availability associated with discharging patients earlier. Increasing bed availability allows more patients with billable diagnostic codes to be admitted, a concept referred to as “throughput.”
This latter concept has been applied to the results of the inpatient diabetes management program at Pitt County Memorial Hospital. The 0.26-day LOS reduction among the 6,876 discharges for patients with diabetes equates to 1,788 days saved per year. These 1,788 days lead to an incremental annual inpatient volume of 350 patients with an average LOS of 5.11 days. Multiplying this incremental inpatient volume by the hospital’s $6,357 revenue margin per patient translates to a throughput value of $2,224,029 for the year. The significance of this value is even greater when expenditures are factored in. Based on the salaries for the Program Director, NCMs, and Program Administrative Office Assistant, as well as consultant fees for the Medical Director and the data management and product services provided by American Healthways, this throughput value yields a 467% return on investment.
Conclusion
The AACE and the American Diabetes Association’s inpatient hyperglycemic management guidelines provide a framework from which organizational initiatives and strategies can be implemented. Through a multidisciplinary team collaboration consisting of ongoing system-wide medical and nursing staff education, policy and procedure development, and outcomes evaluation, hospitals can implement changes in glycemic control regardless of their size or degree of complexity. Although the program described herein is based on roles of the NCM, any model used to impact glycemic management in the hospitalized patient would be expected to improve clinical outcomes and ensure patient safety through multifaceted approaches. The financial implications associated with glycemic control provide opportunities to not only affect the operating margin for institutions but also promote a culture of quality improvement, thereby making aggressive management of hyperglycemia in the hospital a “win-win” situation.
Acknowledgment
We thank Ms Melissa Roupe, RN, MSN, for her dedication and the leadership efforts she has provided to the inpatient diabetes program since its conception.
Affiliations
- Department of Internal Medicine, Division of Endocrinology, Diabetes and Metabolism, Brody School of Medicine at East Carolina University.
- Inpatient Diabetes Program and Care Management Department, Pitt County Memorial Hospital Greenville, North Carolina.
Abbreviations
AACE = American Association of Clinical Endocrinologists; CR-BSI = catheter-related bloodstream infection; ICU = intensive care unit; LOS = length of stay; NCM = nurse case manager.
References
- Donnan PT, Leese GP, Morris AD. Hospitalizations for people with type 1 and type 2 diabetes compared with the nondiabetic population of Tayside, Scotland: a retrospective cohort study of resource use. Diabetes Care. 2000;23:1774- 1779.
- Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: An independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002;87:978-982.
- Williams LS, Rotich J, Qi R, et al. Effects of admission hyperglycemia on mortality and costs in acute ischemic stroke. Neurology. 2002;59:67-71.
- Olveira-Fuster G, Olvera-Marquez P, Carral-Sanlaureano F, Gonzalez-Romero S, Aguilar-Diosdado M, Soriguer-Escofet F. Excess hospitalizations, hospital days, and inpatient costs among people with diabetes in Andalusia, Spain. Diabetes Care. 2004;27:1904-1909.
- Estrada CA, Young JA, Nifong LW, Chitwood WR Jr. Outcomes and perioperative hyperglycemia in patients with or without diabetes mellitus undergoing coronary artery bypass grafting. Ann Thorac Surg. 2003;75:1392-1399.
- Yendamuri S, Fulda GJ, Tinkoff GH. Admission hyperglycemia as a prognostic indicator in trauma. J Trauma. 2003;55:33-38.
- Malmberg K, Norhammar A, Wedel H, Rydén L. Glycometabolic state at admission: important risk marker of mortality in conventionally treated patients with diabetes mellitus and acute myocardial infarction: long-term results from the Diabetes and Insulin-Glucose Infusion in Acute Myocardial Infarction (DIGAMI) study. Circulation. 1999;99:2626-2632.
- Van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in the critically ill patients. N Engl J Med. 2001;345:1359-1367.
- Furnary AP, Gao G, Grunkemeier GL, et al. Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003;125:1007-1021.
- Mesotten D, Van den Berghe G. Clinical potential of insulin therapy in critically ill patients. Drugs. 2003;63:625-636.
- Levetan CS, Salas JR, Wilets IF, Zumoff B. Impact of endocrine and diabetes team consultation on hospital length of stay for patients with diabetes. Am J Med. 1995;99:22-28.
- Koproski J, Pretto Z, Poretsky L. Effects of an intervention by a diabetes team in hospitalized patients with diabetes. Diabetes Care. 1997;20:1553-1555.
- Garber AJ, Moghissi ES, Bransome ED Jr, et al. American College of Endocrinology position statement on inpatient diabetes and metabolic control. Endocr Pract. 2004;10:77-82.
- Clement S, Braithwaite SS, Magee MF, et al. Management of diabetes and hyperglycemia in hospitals. Diabetes Care. 2004;27:553-591.
- Davidson PC, Steed RD, Bode BW. Glucommander: a computer-directed intravenous insulin system shown to be safe, simple, and effective in 120,618 h of operation. Diabetes Care. 2005;28:2418-2423.
- O’Grady NP, Alexander M, Dellinger EP, et al. Guidelines for the prevention of intravascular catheter-related infections. Centers for Disease Control and Prevention. MMWR Recomm Rep. 2002;51(RR-10):1-29.
- Dimick JB, Pelz RK, Consunji R, Swoboda SM, Hendrix CW, Lipsett PA. Increased resource use associated with catheter-related bloodstream infection in the surgical intensive care unit. Arch Surg. 2001;136:229-234.
- National Nosocomial Infections Surveillance System. National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control. 2004; 32:470-485.